Abstract
INTRODUCTION: Chronic lymphocytic leukemia (CLL) is the most common adult leukemia in western countries and its heterogeneous clinical course can be dictated by variable biologic characteristics including chromosomal abnormalities and somatic mutations. Somatic TP53 mutations, with or without deletions of the short arm of chromosome 17 (del17p), have been associated with poor outcomes in CLL, including worse progression free survival, overall survival (OS), chemo-resistance, and risk of Richter's transformation. Although each genetic abnormality carries a negative and usually presents concomitantly, approximately 20-30% of CLL can have TP53 mutations with no del17p. Also, data are lacking regarding the prognostic implications of concurrent TP53 mutations and del17p. The goal of our study was to characterize the prognostic role of TP53 mutations detected by targeted exome sequencing in CLL, with or without del17p genetic aberrations.
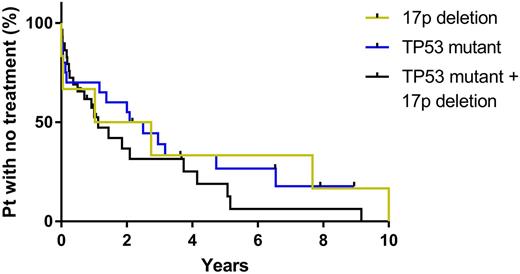
METHODS: Using Total Cancer Care (TCC) Moffitt Cancer Center (MCC) databases, we retrospectively identified CLL patients who had both assessment of TP53 mutationsby next generation sequencing (Genoptix®, Foundation Medicine®, and a 1,321 gene research panel) and del17p status by fluorescence in-situ hybridization (FISH). Clinical variables and disease-related prognostic factors were characterized at the time of diagnosis and annotated using descriptive statistics. Time to the first treatment (TFT) and OS were estimated with the Kaplan-Meier method and compared using log-rank test. Multivariate Cox regression models were used to adjust for age, Rai stage, IgVH mutational status, ZAP70, CD38, and other chromosomal abnormalities including del11q, del13q, and trisomy12. All statistical analyses were performed using SPSS v24.0.
RESULTS: A total of 71 patients were included in the study. The median age was 61 (29-88) years and male patients were 69% (n=49). Twenty-six and eight patients had Rai stage 0/I/II and III/IV, respectively, at the time of diagnosis. IgVH was unmutated in 63% of patients (n=45). A total of 8% (n=6), 38% (n=27), and 54% (n=38) had del17p alone, TP53 mutation alone, or both, respectively. The median number of TP53 mutations in each patient was 1 (1-3) and the most common TP53 mutation was R248Q (n=5) followed by R273C (n=4). Sixty-one patients had additional chromosomal abnormalities; del11q (n=8), del13q (n=33), trisomy12 (n=7), and complex karyotypes (n=13). A total of 83% (n=57) patients received at least one treatment during the follow up. The median TFT in patients with both TP53 mutation and del17p were significantly shorter compared to patients with del17p or TP53 mutation only patients (1.1 vs. 1.9 vs. 3.0 years, p=0.0483), and concurrent TP53 mutation and 17p deletion remained predictive for shorter TFT in multivariate analysis (HR=2.162, 95%CI=1.020-4.580, p=0.044). There was no statistical difference in OS between these three groups (p=0.08716).
CONCLUSIONS: In CLL/SLL patients, concomitant TP53 mutation and del17p is associated with significantly shorter TFT compared to del17p or TP53 mutation independent of Rai stage and other chromosomal abnormalities, which needs prospective validation. Also, these results warrant further study regarding the prognostic impact of different types of dysfunctional TP53 mutation and their allelic burden in the presence and absence of del17p.
Teer: Interpares Biomedicine: Consultancy. Chavez: Incyte: Membership on an entity's Board of Directors or advisory committees; Kite: Speakers Bureau; Abbvie: Speakers Bureau; Janssen: Speakers Bureau. Pinilla-Ibarz: Pfizer: Honoraria, Speakers Bureau; ARIAD: Consultancy, Honoraria; BMS: Honoraria, Speakers Bureau.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal